New thyroid scintigraphy datasets: Construction and benchmark assessment in diagnosis of residual thyroid tissue
640 viewsDOI:
https://doi.org/10.54939/1859-1043.j.mst.88.2023.131-138Keywords:
SPECT image; Thyroid scintigraphy; Computer-Aided Diagnosis; Residual thyroid tissue; Transfer learning.Abstract
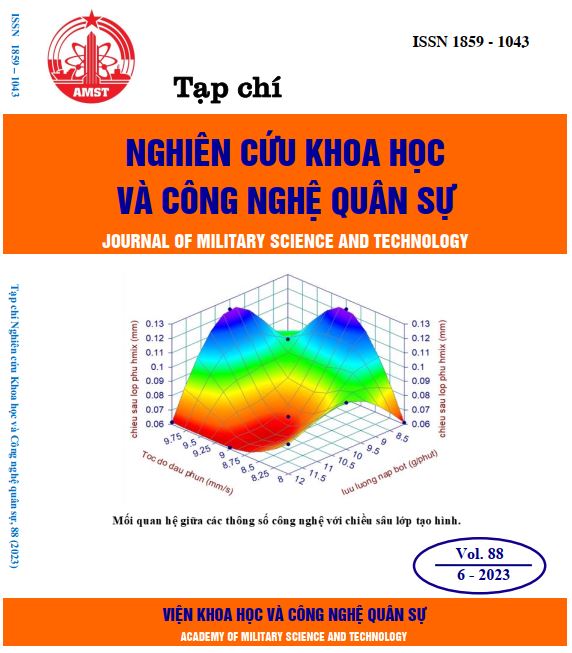
Thyroid scintigraphy, a type of single photon emission computed tomography (SPECT) imaging technique that uses radioactive isotopes to capture images of the thyroid gland, helps detect thyroid abnormalities and diagnosing thyroid cancer. A promising research direction for machine learning applications to assist in diagnosis. Most algorithms for detecting and predicting uptake in the thyroid region rely on proprietary or published datasets with unspecified information. This makes comparing the performance among different methods and developing solutions for various problems challenging. To address this issue, we have constructed two standardized datasets of thyroid scintigraphy images for identifying and quantifying the depth. The purpose of designing the models is to establish a benchmark assessment for developing CADx models on the datasets in the future.
References
[1]. Karssemeijer, N. & te Brake, G. M, “Detection of stellate distortions in mammograms,” IEEE Trans. Med. Imaging, Vol. 15, No. 5, pp. 611–619, (1996). DOI: https://doi.org/10.1109/42.538938
[2]. Mudigonda, N. R., Rangayyan, R. M. & Desautels, J. E. L, “Detection of breast masses in mammograms by density slicing and texture flow-field analysis,” IEEE Trans. Med. Imaging, Vol. 20, No. 12, pp. 1215–1227, (2001). DOI: https://doi.org/10.1109/42.974917
[3]. Liu, S., Babbs, C. F. & Delp, E. J, “Multiresolution detection of spiculated lesions in digital mammograms,” IEEE Trans. IMAGE Process, Vol. 10, No. 6, pp. 874–884, (2001). DOI: https://doi.org/10.1109/83.923284
[4]. Li, L., Clark, R. A. & Thomas, J. A, “Computer-aided diagnosis of masses with full-field digital mammography,” Acad. Radiol, Vol. 9, No. 1, pp. 4–12, (2002). DOI: https://doi.org/10.1016/S1076-6332(03)80290-8
[5]. Baum, F., Fischer, U., Obenauer, S. & Grabbe, E,” Computer-aided detection in direct digital full-field mammography: initial results,” Eur. Radiol, Vol. 12, No. 12, pp. 3015–3017, (2002). DOI: https://doi.org/10.1007/s00330-002-1393-3
[6]. Kim, S. J. et al, “Computer-aided detection in digital mammography: Comparison of craniocaudal, mediolateral oblique, and mediolateral views,” Radiology, Vol. 241, No.3, pp. 695–701, (2006). DOI: https://doi.org/10.1148/radiol.2413051145
[7]. Yang, S. K. et al, “Screening mammography—detected cancers: Sensitivity of a computer-aided detection system applied to fullfield digital mammograms,” Radiology, Vol. 244, No. 1, pp. 104–111, (2007). DOI: https://doi.org/10.1148/radiol.2441060756
[8]. The, J. S., Schilling, K. J., Hoffmeister, J. W. & Mcginnis, R, “Detection of breast cancer with full-field digital mammography and computer-aided detection,” Am. J. Roentgenol, Vol. 192, No. 2, pp. 337–340, (2009). DOI: https://doi.org/10.2214/AJR.07.3884
[9]. Sadaf, A., Crystal, P., Scaranelo, A. & Helbich, T, “Performance of computer-aided detection applied to full-field digital mammography in detection of breast cancers,” Eur. J. Radiol, Vol. 77, No. 3, pp. 457–461, (2011). DOI: https://doi.org/10.1016/j.ejrad.2009.08.024
[10]. Yinxiang Guo et al. “Classification and diagnosis of residual thyroid tissue in SPECT images based on finetuning deep convolutional neural network”. In: Frontiers in Oncology 11 (2021). DOI: https://doi.org/10.3389/fonc.2021.762643
[11]. S. J. Pan and Q. Yang, “A survey on transfer learning,” IEEE Transactions on Knowledge and Data Engineering, vol. 22, no. 10, pp. 1345–1359, (2010). DOI: https://doi.org/10.1109/TKDE.2009.191
[12]. A. Z. Abidin, B. Deng, A. M. DSouza, M. B. Nagarajan, P. Coan et al., “Deep transfer learning for characterizing chondrocyte patterns in phase contrast X-Ray computed tomography images of the human patellar cartilage,” Computers in Biology and Medicine, vol. 95, pp. 24–33, (2018). DOI: https://doi.org/10.1016/j.compbiomed.2018.01.008
[13]. Q. H. Nguyen, B. P. Nguyen, S. D. Dao, B. Unnikrishnan, R. Dhingra et al., “Deep learning models for tuberculosis detection from chest X-ray images,” in Proc. of 26th International Conference on Telecommunications, pp. 381–385, (2019). DOI: https://doi.org/10.1109/ICT.2019.8798798
[14]. P. Hai, N. Thanh, N. Trung, and T. Kien, “Transfer Learning for Disease Diagnosis from Myocardial Perfusion SPECT Imaging”, Comput. Mater. Contin., vol. 73, no. 3, Art. no. 3, (2022), doi: 10.32604/cmc.2022.031027. DOI: https://doi.org/10.32604/cmc.2022.031027
[15]. C. Zhang, K. Qiao, L. Wang, L. Tong, G. Hu et al., “A visual encoding model based on deep neural networks and transfer learning for brain activity measured by functional magnetic resonance imaging,” Journal of Neuroscience Methods, vol. 325, no. 108318, (2019). DOI: https://doi.org/10.1016/j.jneumeth.2019.108318
[16]. Karen Simonyan, Andrew Zisserman, “Very Deep Convolutional Networks for Large-Scale Image Recognition,” arXiv: 1409.1556, (2014).
[17]. Christian Szegedy, Vincent Vanhoucke, Sergey Ioffe, Jonathon Shlens, Zbigniew Wojna, “Rethinking the Inception Architecture for Computer Vision,” arXiv:1512.00567 (2015). DOI: https://doi.org/10.1109/CVPR.2016.308
[18]. Kaiming He, Xiangyu Zhang, Shaoqing Ren, Jian Sun, “Deep Residual Learning for Image Recognition,” arXiv: 1512.03385 (2015).
[19]. François Chollet, “Xception: Deep Learning with Depthwise Separable Convolutions”, arXiv: 1610.02357 (2017) DOI: https://doi.org/10.1109/CVPR.2017.195
[20]. Mark Sandler and Andrew Howard and Menglong Zhu and Andrey Zhmoginov and Liang-Chieh Chen, “MobileNetV2: Inverted Residuals and Linear Bottlenecks”, arXiv: 1801.04381 (2019) DOI: https://doi.org/10.1109/CVPR.2018.00474
[21]. Barret Zoph and Vijay Vasudevan and Jonathon Shlens and Quoc V. Le, “Learning Transferable Architectures for Scalable Image Recognition”, arXiv: 1707.07012 (2018). DOI: https://doi.org/10.1109/CVPR.2018.00907
[22]. Mingxing Tan, Quoc V. Le, “EfficientNet: Rethinking Model Scaling for Convolutional Neural Networks,” arXiv: 1905.11946 (2019).